PENGARUH KOMBINASI ACUPRESSURE dan BRISK WALKING TERHADAP KADAR GULA DARAH PUASA PASIEN DIABETES MELLITUS TIPE II
DOI:
https://doi.org/10.52943/jikeperawatan.v10i2.1627Keywords:
Diabetes Mellitus Type II, Acupressure, Brisk WalkingAbstract
Diabetes mellitus is a disease that has a characteristic sign in the form of an increase in glucose levels exceeding the normal range. The prevalence of diabetes mellitus is increasing significantly. Currently, the management of diet, exercise, and the use of pharmacological therapy are options in the management of diabetes mellitus. In addition to these therapies, there are complementary therapies such as acupressure combined with brisk walking. The purpose of this study was to prove the combination of acupressure and brisk walking intervention in influencing fasting blood glucose levels. This research was a quasi-experimental study with a non-equivalent control group design with pre-test and post-test. This study had 76 respondents with type II diabetes mellitus who were divided into 4 groups and were taken using a consecutive sampling technique. This research was conducted in Bulu Health Center Work Area, Temanggung Regency on April, 7th 2021 – May 9th 2021. The pre-test and post-test difference test used the paired t-test and the Wilcoxon test. The difference test between groups used the Kruskal – Wallis test and continued with the Post Hoc Mann – Whitney test. This study showed that there were significant differences before and after treatment in all groups (p = 0.001). The results of statistical tests also showed that the combination of acupressure and brisk walking was the best treatment for reducing blood glucose levels (p < 0.05) compared to other treatments. Complementary therapy in the form of a acupressure and brisk walking combination is the most effective treatment in reducing blood glucose levels.
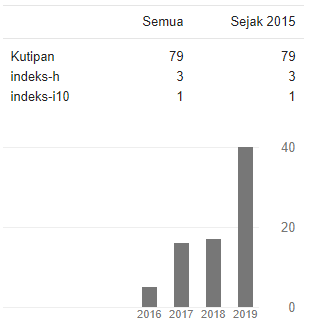
Downloads
References
Arwani, A., Susanto, H., Sawitri, D. R., Widiyati, S., & Daely, L. W. (2019). The Effect of Diabetes Self- Management Education and Support (DSME/S) on Self-Efficacy in Type 2 Diabetes Mellitus Patients. In Journal of Medical Science And clinical Research (Vol. 7, Issue 5, pp. 635–641). https://doi.org/10.18535/jmscr/v7i5.102
Astuti, R. D., Sianturi, M., & Astuti, R. (2017). Efektivitas Active Range of Motion dan Brisk Walking terhadap Kadar Glukosa Darah Pasien Diabetes Melitus di Persadia RS Panti Wilasa Citarum Semarang. Naskah Publikasi. STIKES Telogorejo Semrang, 004. http://ejournal.stikestelogorejo.ac.id/index.php/ilmukeperawatan/article/view/646
Diani, A., & Pulungan, A. B. (2016). Tata laksana Metformin Diabetes Mellitus Tipe 2 pada Anak Dibandingkan dengan obat Anti Diabetes Oral yang lain. Sari Pediatri, 11(6), 395. https://doi.org/10.14238/sp11.6.2010.395-400
Fitrullah, & Rousdy, A. (2017). Effectiveness of Acupressure at the Zusanli (ST-36) Acupoint as a Comfortable Treatment for Diabetes Mellitus: A Pilot Study in Indonesia. JAMS Journal of Acupuncture and Meridian Studies, 10(2), 96–103. https://doi.org/10.1016/j.jams.2016.12.003
Habtamu, W. (2015). Classification, Pathophysiology, Diagnosis and Management of Diabetes Mellitus. Journal of Diabetes & Metabolism, 06(05). https://doi.org/10.4172/2155-6156.1000541
Jamaluddin, M., & Prasetyo, W. M. (2019). Terapi Akupresure Terhadap Keseimbangan Glukosa Darah Pada Pasien Dm Tipe 2 Di Wilayah Kerja Puskesmas Jumpandang Baru Makassar. Media Kesehatan Politeknik Kesehatan Makassar, 14(2), 181. https://doi.org/10.32382/medkes.v14i2.1126
Jateng, D. (2018). Profil Kesehatan Provinsi Jawa Tengah Tahun 2018.
Jumari, Waluyo, A., Jumaiyah, W., & Natashia, D. (2019). Pengaruh Akupresur terhadap Kadar Glukosa Darah Pasien Diabetes Melitus Tipe 2. Journal of Telenursing (JOTING), 1(1), 38–50.
Katsarou, A., Gudbjörnsdottir, S., Rawshani, A., Dabelea, D., Bonifacio, E., Anderson, B. J., Jacobsen, L. M., Schatz, D. A., & Lernmark, A. (2017). Type 1 diabetes mellitus. Nature Reviews Disease Primers, 3, 1–18. https://doi.org/10.1038/nrdp.2017.16
Katzung, B. ., Masters, S. ., & Trevor, A. . (2012). Farmakologi Dasar & Klinik Edisi 12 B (Edisi 12,). Buku Kedokteran EGC.
Kemenkes RI. (2019). Buku Pintar Kader Posbindu. In Direktorat Jendral Pencegahan dan Pengendalian Penyakit Tidak Menular. Direktorat Jendral Pencegahan dan Pengendalian Penyakit Tidak Menular. http://p2ptm.kemkes.go.id/uploads/VHcrbkVobjRzUDN3UCs4eUJ0dVBndz09/2019/03/Buku_Pintar_Kader_POSBINDU.pdf
Khoiriyah, Murbawani, Dian, Etisa, A., & Panunggal, B. (2018). Hubungan Asupan Karbohidrat dan Aktivitas Fisik dengan Prediabetes pada Wanita Dewasa. Universitas Diponegoro.
Khusna, L. U., Sudirman, S., & Suwondo, A. (2019). Implementation Electrical Acupressure Toward Fasting Blood Sugar Levels in Type II Diabetes Mellitus Patients in the Working Area Jepon Community Health Center Blora District. International Journal of Allied Medical Sciences and Clinical Research, 7(3), 657–662.
Kowalk, J. ., Welsh, W., & Mayer, B. (2017). Buku Ajar Patofisiologi. Buku Kedokteran EGC.
Listyarini, A. D., & Fadilah, A. (2017). Brisk Walking Dapat Menurunkan Kadar Glukosa Darah Pada Penderita Diabetes Mellitus Di Desa Klumpit Kecamatan Gebog Kabupaten Kudus. Jurnal Keperawatan Dan Kesehatan Masyarakat Cendekia Utama, 6(2), 10–19. http://jurnal.stikescendekiautamakudus.ac.id/index.php/stikes/article/view/187
Machrina, Y. (2019). Pengaruh Berbagai Model Latihan Terhadap Ekspresi Gen Insr, Reseptor Insulin Otot Skeletal, Resistensi Insulin dan Kadar Gula Darah Pada Tikus Wistar Model Diabetes Melitus Tipe 2 (Issue April). Universitas Sumatera Utara.
Manek, B. . (2019). Pengaruh Pemberian Akupresure SP - 3 Dengan Aromaterapi Kapulaga Terhadap Status Emetogenik dan Emesis Gravidarum Ibu Hamil Trisemester I. Poltekkes Kemenkes Semarang.
Masithoh, R. F., Ropi, H., & Kurniawan, T. (2016). Pengaruh Terapi Akupresur terhadap Kadar Gula Darah pada Pasien Diabetes Melitus Tipe II di Poliklinik Penyakit Dalam RS TK II Soejono Magelang. Journal Of Holistic Nursing Science, 3(2), 26–37. http://journal.ummgl.ac.id/index.php/nursing/article/view/872
Mukhtar, D. (2013). Makrofag Pada Jaringan Adiposa Obes Sebagai Penanda Terjadinya Resistensi Insulin. Jurnal Ilmiah Widya, 3(317), 30–31. http://journal.ummgl.ac.id/index.php/nursing/article/view/872
Nelyanti, D. A., Ta’adi, T., & Anwar, M. C. (2020). The Effectiveness of Acupressure and Smart Gymnastic on Fasting Blood Sugar Levels among Patients with Type II Diabetes Mellitus. International Journal of Nursing and Health Services (IJNHS), 3(6), 687–694. https://doi.org/10.35654/ijnhs.v3i6.368
RI, K. (2018). HASIL UTAMA RISKESDAS 2018.
Sulastri, S., & Arofi, T. M. (2018). Mengendalikan Kadar Glukosa Darah Pasien Diabetes Melitus Tipe 2 Dengan Olah Sehat Lafidzi 21. Jurnal Riset Kesehatan Nasional, 2(1), 1–8. https://doi.org/10.37294/jrkn.v2i1.94
Soelistijo, S. A., Suastika, K., Lindarto, D., Decroli, E., Permana, H., Sucipto, K. W., Kusnadi, Y., Budiman, Ikhsan, R., Sasiarini, L., Sanusi, H., Nugroho, H., & Susanto, H. (2021). Pedoman Pengelolaan dan Pencegahan Diabetes Melitus Tipe 2 Dewasa di Indonesia 2021. In Perkumpulan Endokrinologi Indonesia (p. 46). Perkeni. www.ginasthma.org.
Syafitri, D., Berawati, K. N., & Ichsan, A. A. (2020). Aktivitas Fisik Rutin Sebagai Modulator Sensitivitas Insulin Pada Obesitas. Jurnal Jumantik, 5(1), 9–22.
Terry, C. ., & Weaver, A. (2013). Keperawatan Kritis DeMYSTiFieD. Rapha Publishing.
Triplitt, C. L., & PharmD, C. (2012). Examining the Mechanisms of Glucose Regulation. In The American Journal of Managed Care (Vol. 18, Issue 1 Suppl).
Urbaningrum, V., Sri Endang Pujiastuti, R., & Supriyana, S. (2021). Alternative Yoga Exercise on Fasting Blood Glucose and Cholesterol Levels among Patients with Type 2 Diabetes Mellitus Nursing Student, Postgraduate Program, Master Applied of Health. International Journal of Nursing and Health Services (IJNHS), 4(3), 277–284. https://doi.org/http://doi.org.10.35654/ijnhs.v4i3.445
Widnyana, I. M. G., Agung Senapathi, T. G., Aryabiantara, I. W., Wiryana, M., Sinardja, K., Budiarta, I. G., Aribawa, I. M., Kresna Sucandra, M. A., Parami, P., & Artawan, I. M. (2017). Metabolic Stress Response Attenuate by Oral Glucose Preoperatively in Patient Underwent Major Surgery with General Anesthesia. International Journal of Anesthesiology & Pain Medicine, 03(01), 1–5. https://doi.org/10.21767/2471-982x.100015
Wong, M. . (2018). Holistic Care With Jaripunkture. Wong Publishing.
Zarvasi, A., Ansari Jaberi, A., Negahban Bonabi, T., & Tashakori, M. (2018). Effect of self-acupressure on fasting blood sugar (FBS) and insulin level in type 2 diabetes patients: a randomized clinical trial. Electronic Physician, 10(8), 7155–7163. https://doi.org/10.19082/7155